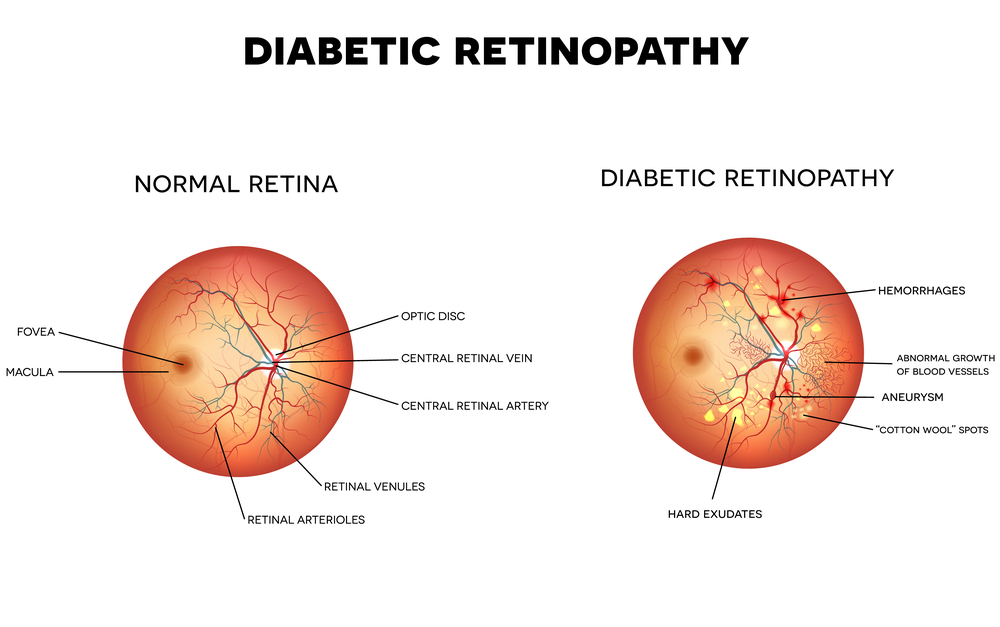
Diabetic retinopathy is one of the most common causes of irreversible blindness in adults with both Type 1 and Type 2 diabetes and is caused by microvascular damage to the retina. Other diabetic eye diseases includes diabetic macular edema, cataract, and glaucoma.
The number of people affected by diabetes, both worldwide and in the United States, is increasing along with the occurrences of diabetic retinopathy. Although these numbers are steadily increasing, only about 60% of people with diabetes have yearly screenings for diabetic retinopathy.
Early detection is paramount to successfully treating patients with diabetic retinopathy to prevent loss of vision and can reduce the risks of blindness by up to 95%. Diabetic retinopathy typically lacks early symptoms. Follow these recommendations to prevent vision loss from diabetic retinopathy if you have diabetes:
- Type 1 diabetes: Get annual screenings beginning five years after the onset of your disease
- Type 2 diabetes: have an examination at the time of diagnosis and every year thereafter
- Take your diabetic medication as prescribed
- Maintain a healthy diet and stay physically active
- Get a comprehensive, dilated eye examination once a year or more frequently based upon exam findings.
Main cause of diabetic retinopathy:
- Chronically high blood sugar from diabetes which leads to damage of the tiny blood vessels in the retina
Diabetic retinopathy can:
- Cause blood vessels in the retina to leak fluid
- Cause hemorrhaging of the eye
- Distort vision or cause total loss of vision
- Cause new abnormal blood vessels to proliferate leading to retinal detachment or a severe form of glaucoma.
Three stages of diabetic retinopathy:
Mild nonproliferative retinopathy shows up in the beginning stages of diabetic retinopathy. At this stage, small areas of balloon-like dilation of blood vessels, also known as micro aneurysms, start to appear along with small spot hemorrhages and cotton wool spots.
Moderate or severe nonproliferative retinopathy – Following mild non-proliferative retinopathy, more micro aneurysms, hemorrhages and cotton wool spots emerge. There is further damage to the retinal blood vessels that may result in reduced blood flow to the surrounding retinal tissue leading to vision loss.
Proliferative diabetic retinopathy – This is the most advanced stage of diabetic retinopathy. Signals sent by the retina for nourishment will essentially cause the retina to produce new blood vessels in an attempt to enhance nourishment. When these new blood vessels are produced, they are typically fragile and tend to break and produce bleeding causing floaters in the retina and vitreous cavity which, in severe cases, lead to vision loss and in some cases permanent blindness.
Detection
There are several tests used to detect diabetic retinopathy depending on the severity of your situation:
- A visual acuity test. This is your basic eye chart test used to check your vision at various distances
- Pupil dilation, where drops are placed to widen the pupils so that your physician may examine your retina and optic nerve
- OCT (optical coherence tomography). Similar to ultrasound, this technique uses light waves instead of sound waves to capture images of tissues inside the body.
- When diabetic retinopathy or DME (diabetic macular edema) is suspected, your physician may perform a fluorescein angiogram to look for leaking or damaged blood vessels. This test is performed by injecting a fluorescent dye into the bloodstream, typically through an arm vein.
Prevention and Treatment
- Diabetic women who become pregnant should have a comprehensive dilated eye exam right away and may require additional exams throughout their pregnancy
- Controlling diabetes is known to slow down the onset or worsening of diabetic retinopathy.
- Diabetic macular edema is treated with laser or anti-VEGF injections or steroid injections.
- With proliferative diabetic retinopathy, laser surgery or anti-VEGF treatment may be recommended to cause abnormal blood vessels to shrink.
- A vitrectomy, surgical removal of the vitreous gel in the center of the eye, is sometimes used to treat severe bleeding into the vitreous.
- Diabetic Retinopathy should be treated by a fellowship trained retinal specialist.
In addition to standard of care treatments, we participate in the National Eye Institute sponsored Diabetic Retinopathy Clinical Research Network as well as other National & International protocols to offer our patients the most advanced treatments available anywhere.
If you have diabetes, you have a significant chance of developing diabetic retinopathy and should have a comprehensive eye examination as soon as possible and annually. If you have been diagnosed with diabetic retinopathy or are concerned that you may have this condition, please call and make an appointment with our experienced fellowship trained retinal specialists at the Fort Lauderdale Eye Institute today. Call 954-741-5555