In 1946, Dr. Harold Ridley of London, was removing a cataract from a patient. A medical student was observing. After surgery, the student asked Dr. Ridley: “You took out the cataract, but you did not replace it with anything. Why not?”. Dr. Ridley patiently explained that that was not the way things were done. But that got him thinking. He had cared for many injured RAF pilots during the war. It was not unusual for him to see a pilot with a fragment of a shattered cockpit inside the pilot’s eye. Surprisingly, this fragment was usually well-tolerated for lengthy periods. Why, he thought, could we not make an intraocular lens out of this plastic material and implant it at the time of surgery? The material was polymethyl methacrylate, which is also known as Plexiglas, Lucite and Perspex. Ridley’s early attempts were usually unsuccessful.
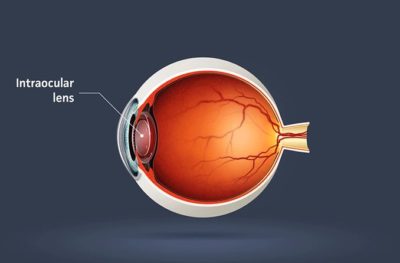
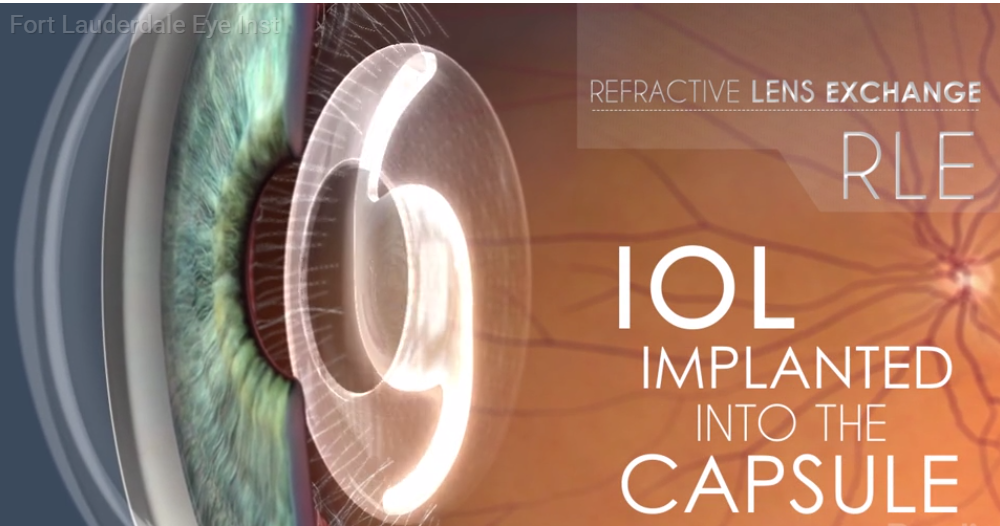
For the next thirty years, many courageous ophthalmologists and their equally brave patients sought to improve the safety and quality of implants. A major breakthrough came in the late seventies with Doctors Binkhorst and Worst in Europe and Dr. Shearing in America and many others. They began putting their implants “in the bag”. Instead of removing the entire cataract, they scooped out the inside of the lens, leaving the capsule, the outer envelope of the lens intact. They then implanted their lenses into this cavity which gave the lens implant a natural support system. Success dramatically improved.
While this was going on, Dr. Charles Kelman, was developing phacoemulsification, a radically new method of removing cataracts. In this technique, a small probe is passed into the eye and ultrasonic vibrations are used to break up the cataract into tiny particles, easily removed through the small probe. This allowed the cataract to be removed through a small opening. This left a problem: the opening was too small to allow the insertion of the intraocular lens, so wound had to be enlarged.
Enter the foldable implant. First made of silicone, these lenses could be folded in half, inserted through a small opening, and then unfolded inside the eye to their original shape, all this taking place “within the bag”. Implant materials and designs continued to improve through the late 20th century and early 21st century. Implants were developed that could be rolled instead of just folded, allowing insertion through smaller and smaller incisions.
The next major leap forward was the development of specialty lenses with optics that could allow the patient to see both distance and near through the same lens. There are several varieties of these implants available from different companies.
Some patients have a large amount of astigmatism. The cornea is the clear window at the front of the eye. Often, it is shaped more like a football rather than a basketball. This defect can be optically corrected with proper glasses. After cataract surgery, the shape of the cornea does not change much. Therefore, patients with astigmatism will still need glasses for distance and near to see clearly. Enter the toric implant. This implant is constructed with astigmatism of various powers built in, and allows clear vision, often without glasses.
The 65 year history of lens implants has been strewn with failure and partial success. Today, cataract surgery with implantion of an intraocular lens is the safest operation in the world, boasting more than a 98% success rate. We owe a lot to those surgeons and their patients who were willing to “take a chance” on something new.